Navigating New Jersey's Medicaid Regulatory Landscape
This video describes how New Jersey’s Medicaid program (NJ FamilyCare) is administered by the Division of Medical Assistance & Health Services (DMAHS) and how EVV mandates, home care regulations, provider licensing, managed care organization (MCO) contracts and state oversight interact. It also highlights how CareSmartz360 supports compliance across these regulatory layers.
Who we empower every day
By Role- Agency Owners – Build operations aligned with DMAHS, MCO partners, EVV requirements and managed care workflows
- Supervisors – Ensure staff works under compliant contracts, regulated workflows and service authorizations
- Care Managers – Coordinate delivery of services within Medicaid rules, care plans and capture systems
- Billers – Submit claims under appropriate Medicaid/MCO protocols backed by EVV-captured data
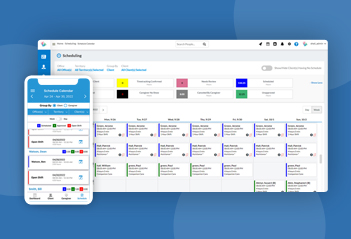
- Schedulers – Plan shifts according to authorization, hours, EVV capture and payer rules
- Caregivers – Work with agencies that comply with regulation, capture visits and uphold standards
- On-Call Coordinators – Manage dynamically within regulatory and payer-model constraints
In New Jersey, agencies operate under managed-care contracts, EVV mandates and payer rules; integration across scheduling, capture, billing and documentation is critical. Choosing a full-stack platform like CareSmartz360 supports regulatory alignment and operational resilience.
 AI Hub
AI Hub